At a time when the nation’s healthcare providers are under increasing stress, a newly published article in JAMA Surgery examines the risk factors contributing to suicide in their professions.
Yisi Daisy Ji, DMD18, clinical fellow in Oral and Maxillofacial Surgery at Massachusetts General Hospital (MGH) and lead author of the manuscript, “Assessment of Risk Factors for Suicide Among US Health Care Professionals,” described why it was important to delve deeper into this topic.

Ji and her co-authors Faith Robertson, MD, MSc, resident in Neurosurgery at Massachusetts General Hospital (MGH); Nisarg Patel, DMD18, clinical fellow in Oral and Maxillofacial Surgery at University of California, San Francisco; Zachary Peacock, DMD, MD, assistant professor of Oral and Maxillofacial Surgery at HSDM/MGH; and Cory Resnick, MD, DMD, assistant professor of Oral and Maxillofacial Surgery at HSDM/MGH, studied 170,030 individuals in healthcare roles (surgeons, non-surgeon physicians, and dentists) who died by suicide.
Of these individuals, they found that those who died by suicide were more likely to have problems with their jobs, physical health, and civil legal issues compared with individuals in the general population who died by suicide. Additionally, individuals of Asian or Pacific Islander ancestry were at higher risk. A direct comparison between surgeons and non-surgeon physicians revealed that surgeons had a higher risk of suicide if they were older, male, married, or currently receiving treatment for mental illness.

While the study was undertaken well before the COVID-19 pandemic, Ji notes the additional stress healthcare professionals are now under could be another factor to consider.
“There are new challenges that we’ve never faced before, including new environments and novel challenges presented by COVID. Providers are being asked to work in different environments to treat COVID patients. Many physicians and residents have been task-shifted from their original service onto COVID services. For example, an oncology fellow might be moved to the COVID service. In addition, social distancing has precluded many of the supports that healthcare providers might rely on,” she said.
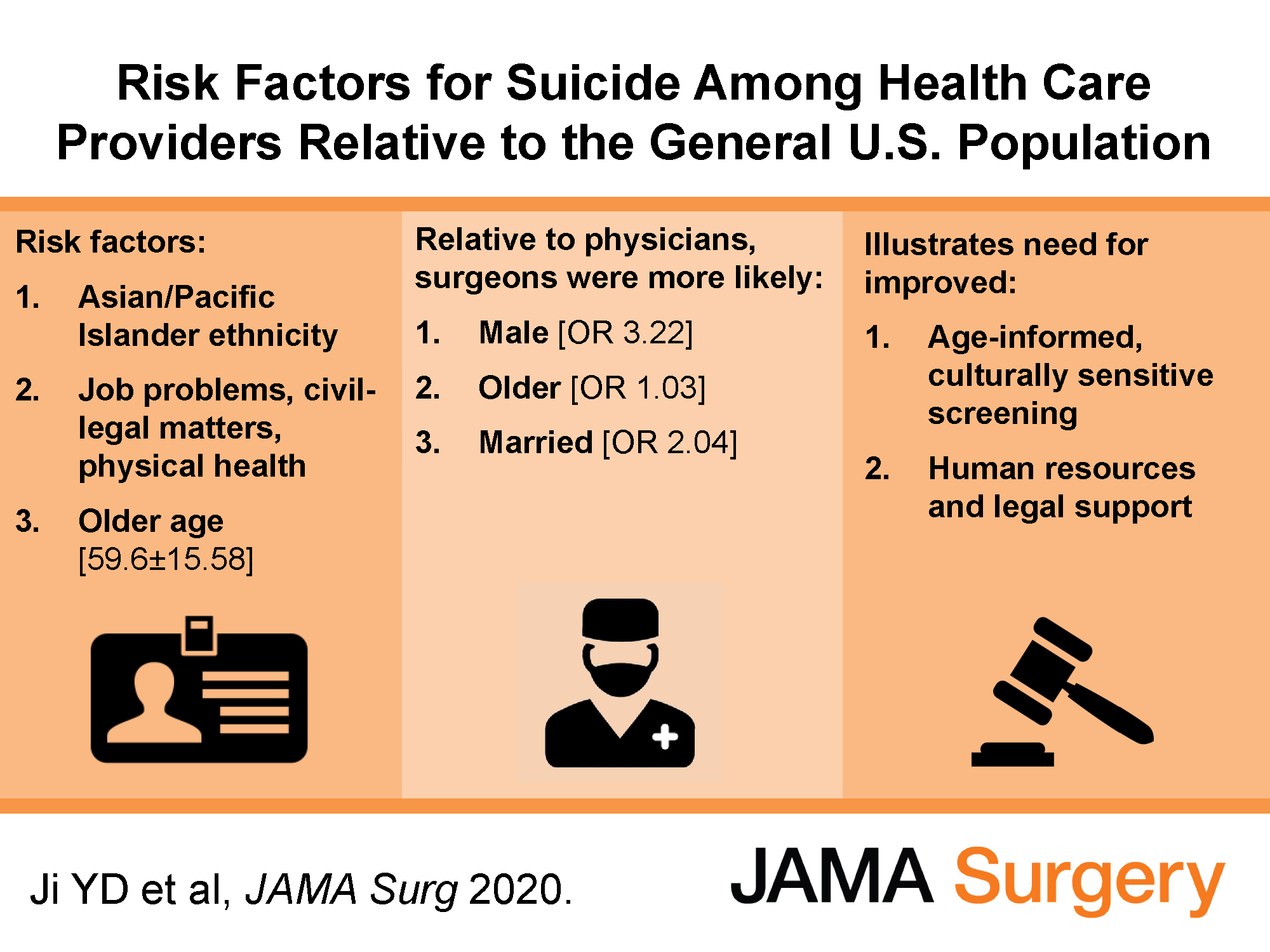 The study’s results may be useful to hospital and healthcare training programs and lead to improvements in the detection of burnout and the development of suicide prevention interventions among health care professionals.
The study’s results may be useful to hospital and healthcare training programs and lead to improvements in the detection of burnout and the development of suicide prevention interventions among health care professionals.
“We hope that the findings will help both residency program directors and health systems better identify those at higher risk and prevent suicides from happening. This is not to say that we should only focus on these individuals, as all healthcare providers might benefit from screening, but that further consideration might be needed in addressing these individuals who have fallen through existing mental health screens/supports,” Ji said.